Clinical Outcomes for Localized Prostate Cancer
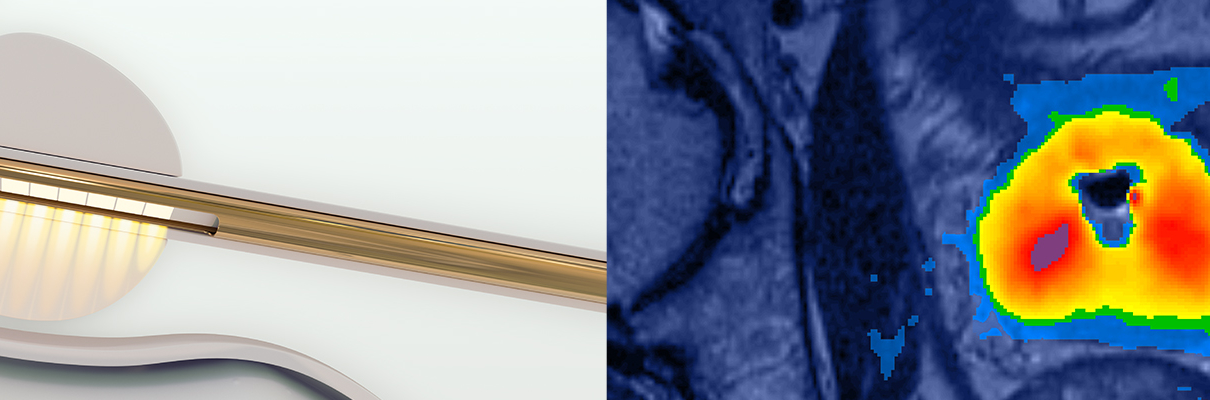
Primary Evidence of Safety & Efficacy: TACT Pivotal Study (n=115)
Klotz et al, “MRI-guided transurethral ultrasound ablation of prostate cancer,” The Journal of Urology (2020)
Primary TACT publication demonstrating effective tissue ablation and PSA reduction with low rates of toxicity and residual disease.
Eggener et al, AUA 2020 Annual Meeting (abstract PD17-02) “Pivotal trial of MRI-guided transurethral ultrasound ablation in men with localized prostate cancer: two-year follow-up,”
Preliminary 2y outcomes show stable PSA, no new safety events, and continued recovery of erectile and urinary function. By 2y, 7% of men underwent additional therapy for prostate cancer.
Sundaram et al, “MRI-guided transurethral ultrasound ablation of localized prostate cancer: preliminary experience from a single center in a prospective, multi-center, single-arm clinical trial,” Journal of Vascular and Interventional Radiology (2020)
Single-center TACT experience from Vanderbilt University Medical Center.
Durability of Outcomes and Feasibility of Salvage Treatment: Phase I Safety & Precision Study (n=30)
Chin et al, “Magnetic resonance imaging-guided transurethral ultrasound ablation of prostate tissue in patients with localized prostate cancer: A prospective Phase 1 clinical trial,” European Urology (2016)
Primary Phase I publication demonstrating favourable safety and quality of life outcomes to 12 months. PSA and biopsy outcomes in accordance with 90% prostate treatment plan.
Bonekamp et al, “Twelve-month prostate volume reduction after MRI-guided transurethral ultrasound ablation of the prostate,” European Radiology (2018)
Supporting publication focused on imaging findings including 88% prostate volume reduction in accordance with treatment plan.
Nair et al, “MRI-guided transurethral ultrasound ablation in patients with localized prostate cancer: Three year outcomes of a prospective Phase I study,” BJU International (2020)
Consistent biopsy results at 3 years compared to those at 12 months. No new serious or severe adverse events to 3 years. Urinary, bowel function remained stable from 12 months, and erectile function recovered by 1 year and stable to 3 years.
Chin et al, “Five-year Outcomes from a Prospective Phase I Study of MRI-guided Transurethral Ultrasound Ablation in Men with Localized Prostate Cancer,” AUA 2020 Annual Meeting (abstract PD17-03) & EAU 2020 Virtual Congress (abstract 884).
5 year outcomes demonstrate durability of the data. Patients without residual disease are stable on PSA to 5 years, and continue to see favorable safety and quality of life. Patients with residual disease progressed as expected and some underwent salvage treatment for their prostate cancer. Residual disease was feasible to detect and radical, salvage options were safe and effective. 100% cancer specific survival and 97% overall survival at 5 years.
Nair et al, “Salvage open radical prostatectomy for recurrent prostate cancer following MRI-guided transurethral ultrasound ablation (TULSA) of the prostate: feasibility and efficacy,” Scandinavian Journal of Urology (2020)
Report of post-TULSA salvage prostatectomy experience. Procedure is feasible and less complicated than post-radiation salvage prostatectomy.
Hatiboglu et al, “Magnetic resonance imaging‑guided transurethral ultrasound ablation of prostate tissue in patients with localized prostate cancer: single‑center evaluation of 6‑month treatment safety and functional outcomes of intensified treatment parameters,” World Journal of Urology (2019)
Compares single-center patients under Phase I versus TACT treatment planning protocols. TACT protocol shows improved efficacy with similar favorable safety profile.
Demonstrating Feasibility in other Prostate Disease States
Benign Prostatic Hyperplasia (BPH), Relief of Lower Urinary Tract Symptoms (LUTS)
Elterman et al, “Relief of lower urinary tract symptoms after MRI-guided transurethral ultrasound ablation (TULSA) for localized prostate cancer: Subgroup analyses in patients with concurrent cancer and benign prostatic hyperplasia,” Journal of Endourology (2020)
BPH sub-group analysis of Phase I cancer study. IPSS improved significantly by 58% from 16.1 to 6.3 at 12 months (p=0.003), with at least a moderate (≥6 points) reduction in 8/9 patients.
Vittala et al, “Transurethral ultrasound therapy for benign prostatic obstruction in humans,” EAU 2020 Virtual Congress (abstract 648).
Initial outcomes of prospective study of TULSA in men with BPH. IPSS decreased from 17.7 to 4.6 at 3 months, with no adverse events on sexual or bowel function.
Radio-Recurrent Localized Prostate Cancer: Phase I Study of Salvage TULSA (n=11)
Anttinen et al, “Salvage MRI-guided TULSA for localized radio-recurrent prostate cancer: 12-month functional and oncological results,” European Urology Open Science (2020)
Initial outcomes of TULSA for salvage ablation in men with radio-recurrent localized prostate cancer.
Palliation of Symptomatic Locally Advanced Prostate Cancer: Phase I Study of Palliative TULSA (n=10)
Anttinen et al, “Palliative MRI-guided transurethral ultrasound ablation for symptomatic locally advanced prostate cancer,” Scandinavian Journal of Urology (2020)
Palliation of urinary retention and intractable hematuria in patients with locally advanced prostate cancer.
Validation of Treatment Effect, Treat-and-Resect Studies (n=19, 3 studies)
University of Turku, Lesion-Targeted Ablation with Prostatectomy at 3 Weeks (n=6)
Anttinen et al, “Feasibility of MRI-guided transurethral ultrasound for lesion-targeted ablation of prostate cancer,” Scandinavian Journal of Urology (2019)
Treat-and-resect study (n=6), TULSA followed by prostatectomy at 3 weeks, lesion-targeted ablation, including demonstration of histological efficacy of TULSA in men with high-risk disease.
Anttinen et al, “Histopathological evaluation of prostate specimens after thermal ablation may be confounded by the presence of thermally-fixed cells,” International Journal of Hyperthermia (2019)
Case study of the above trial, demonstrating the presence of “thermally fixed” cells which can appear normal on standard histology but are in fact non-viable.
Makela et al, “Acute and subacute prostate MRI findings after MRI-guided transurethral ultrasound ablation of prostate cancer,” Acta Radiologica (2020)
MRI findings in the first three weeks after TULSA treatment for men in the Turku treat-and-resect study and determine optimal parameters for post-treatment imaging.
Sunnybrook Hospital, First-in-Man Treat-and-Resect Studies (n=13, 2 studies)
Ramsay et al, “Evaluation of focal ablation of MRI-defined prostate cancer using MRI-controlled transurethral ultrasound therapy with prostatectomy as the reference standard,” Journal of Urology 197: 255-261 (2017)
Second treat-and-resect study (n=5), TULSA followed by prostatectomy on the same day, lesion-targeted ablation.
Chopra et al, “MR Imaging-controlled transurethral ultrasound therapy for conformal treatment of prostate tissue: Initial feasibility in humans,” Radiology 265(1): 303-13 (2012)
First-in-man study (n=8), TULSA followed by prostatectomy on the same day, not targeting cancer.
Review
Galgano et al, “MR-guided high-intensity directional ultrasound ablation of prostate cancer”, Curr Urol Rep (2021)
Arcot et al, “Does MRI-guided TULSA provide a targeted approach to ablation?”, Nat Rev Urol (2020)
Sundaram et al, “Therapeutic ultrasound and prostate cancer,” Semin Intervent Radiol (2017)
Pre-Clinical
Burtnyk et al, “Magnetic resonance image guided transurethral ultrasound prostate ablation: A preclinical safety and feasibility study with 28-day follow-up,” The Journal of Urology 193: 1669-1675 (2015)
Sammet et al, “Cavernosal nerve functionality evaluation after magnetic resonance imaging-guided transurethral ultrasound treatment of the prostate,” World Journal of Radiology 7(12): 521-530 (2015)
Siddiqui et al, “MRI-guided transurethral ultrasound therapy of the prostate gland using real-time thermal mapping: initial studies”, Urology 76(6): 1506-11 (2010)
Chopra et al, “MRI-controlled transurethral therapy for localized prostate cancer”, International Journal of Hyperthermia 26(8): 804-21 (2010)
Chopra et al, “Analysis of the spatial and temporal accuracy of heating in the prostate gland using transurethral ultrasound therapy and active MR temperature feedback,” Physics in Medicine and Biology 54: 2615-33 (2009)
Chopra et al, “MRI-compatible transurethral ultrasound system for the treatment of localized prostate cancer using rotational control,” Medical Physics 35: 1346-57 (2008)
Boyes et al, “Prostate tissue analysis immediately following magnetic resonance imaging guided transurethral ultrasound thermal therapy,” The Journal of Urology 178: 1080-5 (2007)
Tang K et al, “Conformal thermal therapy using planar ultrasound transducers and adaptive closed-loop MR temperature control: demonstration in gel phantoms and ex vivo tissues,” Physics in Medicine and Biology, 52: 2905-19 (2007)
Technical Development
Suomi et al, “Transurethral ultrasound therapy of the prostate in the presence of calcifications: A simulation study,” Medical Physics (2018)
N’Djin et al, “Investigation of power and frequency for 3D conformal MRI-controlled transurethral ultrasound therapy with a dual frequency multi-element transducer,” Int J Hyperthermia 28(1): 87-104 (2012)
N’Djin et al, “Coagulation of human prostate volumes with MRI-controlled transurethral ultrasound therapy: results in gel phantoms,” Medical Physics 39(7): 4524-36 (2012)
Burtnyk et al, “Simulation study on the heating of the surrounding anatomy during transurethral ultrasound prostate therapy: A 3D theoretical analysis of patient safety”, Medical Physics 37(6): 2862-75 (2010)
Burtnyk et al, “3D Conformal MRI-controlled transurethral ultrasound prostate therapy: validation of numerical simulations and demonstration in tissue-mimicking gel phantoms”, Physics in Medicine and Biology 55(22):6817-39 (2010)
Burtnyk et al, “Quantitative analysis of 3D conformal MRI-guided transurethral ultrasound therapy of the prostate: theoretical simulations,” International Journal of Hyperthermia 25(2): 116-31 (2009)
Chopra et al, “Analysis of factors important for transurethral ultrasound prostate heating using MR temperature feedback,” Physics in Medicine and Biology 51: 827-44 (2006)
Chopra et al, “Method for MRI-guided conformal thermal therapy of prostate with planar transurethral ultrasound heating applicators,” Physics in Medicine and Biology 50: 4957-75 (2005)
Galgano S. et al, “MR-Guided High-Intensity Directional Ultrasound Ablation of Prostate Cancer,” Current Urology Reports (2021)
Purpose of Review
Recent Findings
Summary
Kayano P. and Klotz L., “Current evidence for focal therapy and partial gland ablation for organ-confined prostate cancer: systematic review of literature published in the last 2 years,” Current Opinion in Urology (2021)
Purpose of review
The shift in the diagnostic algorithm for prostate cancer to early imaging with mpMRI has resulted in many patients being diagnosed with small volume, apparently unilateral, clinically significant cancers. In these patients, a minimally invasive, nonmorbid intervention is appealing. The aim of this study was to review data reported within the last 2 years on focal therapy and partial gland ablation for organ-confined prostate cancer.
Recent findings
High-intensity focal ultrasound, focal cryotherapy, photodynamic therapy, irreversible electroporation and focal laser ablation, have been used as treatment modalities for localized prostate cancer treatment. The reported oncologic outcomes vary widely and makes comparisons challenging. All the focal therapies report low rates of complications, and high rates of continence and erectile function preservation. The most common adverse events are hematuria, urinary retention and urinary tract infections. During this period, the initial results of several new technologies including MRI-guided transurethral ultrasound ablation were published.
Summary
Focal therapy and partial gland ablation for organ-confined prostate cancer is an option for patients with intermediate-risk disease because of its low complication profile and preservation of QOL. Trials comparing the outcome of different focal therapy technologies have not been carried out, and the existing evidence does not point to one approach being clearly superior to others. Long-term oncologic outcome is lacking. Despite this, for men with unilateral intermediate-risk prostate cancer whose disease is often relatively indolent, focal therapy is an appealing option.
Klotz et al, “MRI-guided transurethral ultrasound ablation of prostate cancer,” The Journal of Urology (2020)
Purpose:
Magnetic resonance imaging-guided transurethral ultrasound ablation uses directional thermal ultrasound under magnetic resonance imaging thermometry feedback control for prostatic ablation. We report 12-month outcomes from a prospective multicenter trial (TACT).
Materials and Methods:
A total of 115 men with favorable to intermediate risk prostate cancer across 13 centers were treated with whole gland ablation sparing the urethra and apical sphincter. The co-primary 12-month endpoints were safety and efficacy.
Results:
In all, 72 (63%) had grade group 2 and 77 (67%) had NCCN® intermediate risk disease. Median treatment delivery time was 51 minutes with 98% (IQR 95–99) thermal coverage of target volume and spatial ablation precision of ±1.4 mm on magnetic resonance imaging thermometry. Grade 3 adverse events occurred in 9 (8%) men. The primary endpoint (U.S. Food and Drug Administration mandated) of prostate specific antigen reduction ≥75% was achieved in 110 of 115 (96%) with median prostate specific antigen reduction of 95% and nadir of 0.34 ng/ml. Median prostate volume decreased from 37 to 3 cc. Among 68 men with pretreatment grade group 2 disease, 52 (79%) were free of grade group 2 disease on 12-month biopsy. Of 111 men with 12-month biopsy data, 72 (65%) had no evidence of cancer. Erections (International Index of Erectile Function question 2 score 2 or greater) were maintained/regained in 69 of 92 (75%). Multivariate predictors of persistent grade group 2 at 12 months included intraprostatic calcifications at screening, suboptimal magnetic resonance imaging thermal coverage of target volume and a PI-RADS™ 3 or greater lesion at 12-month magnetic resonance imaging (p <0.05).
Conclusions:
The TACT study of magnetic resonance imaging-guided transurethral ultrasound whole gland ablation in men with localized prostate cancer demonstrated effective tissue ablation and prostate specific antigen reduction with low rates of toxicity and residual disease.
Anttinen et al, “Salvage MRI-guided TULSA for Localized Radiorecurrent Prostate Cancer: 12-Month Functional and Oncological Results,” European Urology Open Science (2020)
Background:
Up to half of all men who undergo primary radiotherapy for localized prostate cancer (PCa) experience local recurrence.
Objective:
To evaluate the safety and early functional and oncological outcomes of salvage magnetic resonance imaging–guided transurethral ultrasound ablation (sTULSA) for men with localized radiorecurrent PCa.
Design, setting, and participants:
This prospective, single-center phase 1 study (NCT03350529) enrolled men with biopsy-proven localized PCa recurrence after radiotherapy. Multiparametric magnetic resonance imaging (mpMRI) and 18F prostate-specific membrane antigen-1007 ( 18F PSMA-1007) positron emission tomography (PET)-computed tomography (CT) were used to confirm organ-confined disease localization. Patients underwent either whole-gland or partial sTULSA, depending on their individual tumor characteristics.
Outcome measurements and statistical analysis:
Patients were followed at 3-mo intervals. Adverse events (AEs, Clavien-Dindo scale), functional status questionnaires (Expanded Prostate Cancer Index [EPIC]-26, International Prostate Symptom Score, International Index of Erectile Function-5), uroflowmetry, and prostatespecific antigen (PSA) were assessed at every visit. Disease control was assessed at 1 yr using mpMRI and 18F-PSMA-1007 PET-CT, followed by prostate biopsies.
Results and limitations:
Eleven patients (median age 69 yr, interquartile range [IQR] 68–74) underwent sTULSA (3 whole-gland, 8 partial sTULSA) and have completed 12-mo follow-up. Median PSA was 7.6 ng/ml (IQR 4.9–10) and the median time from initial PCa diagnosis to sTULSA was 11 yr (IQR 9.5–13). One grade 3 and three grade 2 AEs were reported, related to urinary retention and infection. Patients reported a modest degradation in functional status, most significantly a 20% decline in the EPIC-26 irritative/obstructive domain at 12 mo. A decline in maximum flow rate (24%) was also observed. At 1 yr, 10/11 patients were free of any PCa in the targeted ablation zone, with two out-of-field recurrences. Limitations include the nonrandomized design, limited sample size, and shortterm oncological outcomes.
Conclusions:
sTULSA appears to be safe and feasible for ablation of radiorecurrent PCa, offering encouraging preliminary oncological control.
Patient summary:
We present safety and 1-yr functional and oncological outcomes of magnetic resonance imaging–guided transurethral ultrasound ablation (TULSA) as a salvage treatment for local prostate cancer recurrence after primary radiation. Salvage TULSA is safe and shows the ability to effectively ablate prostate cancer recurrence, with acceptable toxicity. © 2020 The Authors. Published by Elsevier B.V. on behalf of European Association of Urology. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Anttinen et al, “Palliative MRI-guided transurethral ultrasound ablation for symptomatic locally advanced prostate cancer,” Scandinavian Journal of Urology (2020)
Purpose:
Locally advanced prostate cancer can cause bladder outlet obstruction, gross hematuria and frequent hospitalization. While these complications are commonly treated by palliative transurethral resection of the prostate, the improvement is often insufficient. The purpose of this study was to evaluate the safety and feasibility of MRI-guided transurethral ultrasound ablation as an alternative palliative treatment option (pTULSA) for men suffering from symptomatic locally advanced prostate cancer.
Methods:
This prospective, phase one study included 10 men in need of palliative surgical intervention due to urinary retention and gross hematuria caused by locally advanced prostate cancer. Patients were followed for 1 year at 3-month intervals. Time without catheter, time without hematuria, reduction in hospitalization time, and adverse events were measured.
Results:
Ten patients with locally advanced prostate cancer were enrolled, all having continuous catheterization due to urinary retention and nine had gross hematuria before treatment. At 1 week postpTULSA five patients were catheter-free. At last follow-up catheter-free and gross hematuria-free rates were 70% and 100%, respectively. Average hospitalization time from local complications reduced from 7.3 to 1.4 days in the 6 months before and after pTULSA. No> Grade 2 treatment related adverse events were reported, with all five being urinary tract infections.
Conclusions:
pTULSA appears safe and feasible for palliative ablation of locally advanced prostate cancer. The therapy seems to accomplish long-term hematuria control, can relieve bladder outlet obstruction in selected patients, and seems to reduce the burden of hospitalization due to local complications.
Trial Registration Number: NCT03350529
Elterman et al, “Relief of Lower Urinary Tract Symptoms after MRI-Guided Transurethral Ultrasound Ablation (TULSA) for localized prostate cancer: Subgroup Analyses in Patients with concurrent cancer and Benign Prostatic Hyperplasia,” Journal of Endourology (2020)
Background:
MRI-guided transurethral ultrasound ablation (TULSA) offers minimally invasive thermal ablation of benign and malignant prostate tissue, using directional high-intensity ultrasound and real-time, magnetic resonance thermometry feedback control. Feasibility of TULSA for alleviating lower urinary tract symptoms (LUTSs) associated with benign prostatic hyperplasia (BPH) is retrospectively assessed in a subgroup of men from a localized prostate cancer study who also had LUTSs.
Patients and Methods:
TULSA was used to ablate 90% of the prostate gland in 30 men with localized prostate cancer, without plans to spare ejaculatory ducts. Mean ± standard deviation treatment time was 37 ± 10 minutes. Retrospective analysis was conducted on a subpopulation of nine patients who also suffered from LUTSs (International Prostate Symptom Score [IPSS] ≥ 12 at baseline) as well as a smaller subgroup of five patients with IPSS >12 and peak urinary flow (Qmax) <15 mL/second. Urinary symptom relief, continence, and erectile function were assessed using IPSS, International Index of Erectile Function (IIEF), and uroflowmetry.
Results:
At 12 months post-TULSA, IPSS improved significantly by 58% to 6.3 ± 5.0 (p = 0.003), with at least a moderate (≥6 points) reduction in eight of nine patients. IPSS quality of life improved in eight of nine patients. Erectile function (IIEF-EF) remained stable from 14.6 ± 9.3 at baseline to 15.7 ± 9.0 at 12 months. The proportion of patients with erections sufficient for penetration (IIEF Q2 ≥2) was unchanged. Full urinary continence (pad free and leak free) was achieved at 12 months in all patients. In five men who suffered from more severe symptoms, Qmax increased from 11.6 ± 2.6 mL/second to 22.5 ± 14.2 mL/second at 12 months (p = 0.126). Perfused prostate volume, measured on MRI, decreased 70% to 13.6 ± 4.6 mL (p = 0.003) at 12 months. All adverse events were mild to moderate (Common Terminology Criteria for Adverse Events [CTCAE] Grade 1–2) with no serious events reported.
Conclusions:
This retrospective analysis demonstrates promising safety and feasibility of TULSA to relieve LUTSs, with improvement in IPSS comparable with modern, minimally invasive surgical therapies. Larger controlled studies with BPH-specific ablation plans in men seeking treatment for LUTSs are warranted.
Sundaram et al, “MRI-guided transurethral ultrasound ablation of localized prostate cancer: preliminary experience from a single center in a prospective, multi-center, single-arm clinical trial,” Journal of Vascular and Interventional Radiology (2020)
Abstract
Makela P. et al, “Acute and subacute prostate MRI findings after MRI-guided transurethral ultrasound ablation of prostate cancer,” Acta Radiologica (2020)
Background
Magnetic resonance imaging (MRI)-guided transurethral ultrasound ablation (TULSA) is an emerging method for treatment of localized prostate cancer (PCa). TULSA-related subacute MRI findings have not been previously characterized.
Purpose
To evaluate acute and subacute MRI findings after TULSA treatment in a treat-and-resect setting.
Material and Methods
Six men with newly diagnosed MRI-visible and biopsy-concordant clinically significant PCa were enrolled and completed the study. Eight lesions classified as PI-RADS 3–5 were focally ablated using TULSA. One- and three-week follow-up MRI scans were performed between TULSA and robot-assisted laparoscopic prostatectomy.
Results
TULSA-related hemorrhage was detected as a subtle T1 hyperintensity and more apparent T2 hypointensity in the MRI. Both prostate volume and non-perfused volume (NPV) markedly increased after TULSA at one week and three weeks after treatment, respectively. Lesion apparent diffusion coefficient values increased one week after treatment and decreased nearing the baseline values at the three-week MRI follow-up.
Conclusion
The optimal timing of MRI follow-up seems to be at the earliest at three weeks after treatment, when the post-procedural edema has decreased and the NPV has matured. Diffusion-weighted imaging has little or no added diagnostic value in the subacute setting.
Nair et al, “MRI-Guided Transurethral Ultrasound Ablation in Patients with Localized Prostate Cancer: Three Year Outcomes of a Prospective Phase I Study,” BJU International (2020)
Objectives
To report the 3‐year follow‐up of a Phase I study of magnetic resonance imaging (MRI)‐guided transurethral ultrasound ablation (TULSA) in 30 men with localised prostate cancer. Favourable 12‐month safety and ablation precision were previously described.
Patients and Methods
As a mandated safety criterion, TULSA was delivered as near whole‐gland ablation, applying 3‐mm margins sparing 10% of peripheral prostate tissue in 30 men. After 12‐month biopsy and MRI, biannual follow‐up included prostate‐specific antigen (PSA), adverse events (AEs), and functional quality‐of‐life assessment, with repeat systematic biopsy at 3 years.
Results
A 3‐year follow‐up was completed by 22 patients. Between 1 and 3 years, there were no new serious or severe AEs. Urinary and bowel function remained stable. Erectile function recovered by 1 year and was stable at 3 years. The PSA level decreased 95% to a median (interquartile range) nadir of 0.33 (0.1–0.4) ng/mL, stable to 0.8 (0.4–1.6) ng/mL at 3 years. Serial biopsies identified clinically significant disease in 10/29 men (34%) and any cancer in 17/29 (59%). By 3 years, seven men had recurrence (four histological, three biochemical) and had undergone salvage therapy without complications (including six prostatectomies). At 3 years, three of 22 men refused biopsy, and two of the 22 (9%) had clinically significant disease (one new, one persistent). Predictors of salvage therapy requirement included less extensive ablation coverage and higher PSA nadir.
Conclusion
With 3‐year Phase I follow‐up, TULSA demonstrates safe and precise ablation for men with localised prostate cancer, providing predictable PSA and biopsy outcomes, without affecting functional abilities or precluding salvage therapy.
Arcot R. and Polascik T., “Does MRI-guided TULSA provide a targeted approach to ablation?” Nature Reviews Urology (2020)
Abstract
MRI-guided transurethral ultrasound ablation is an exciting, minimally invasive technology with the potential to provide targeted ablation of prostate cancer tissue. At 3 years, functional outcomes remain good with 76% remaining free from salvage treatment. Future studies using a focal approach may provide evidence for widespread uptake of this technology. Refers to Nair, S. M. et al. Magnetic resonance imaging-guided transurethral ultrasound ablation in patients with localised prostate cancer: 3-year outcomes of a prospective phase I study. BJU Int. https://doi.org/10.1111/bju.15268 (2020).
Nair et al, “Salvage open radical prostatectomy for recurrent prostate cancer following MRI-guided transurethral ultrasound ablation (TULSA) of the prostate: feasibility and efficacy,” Scandinavian Journal of Urology (2020)
Introduction:
MRI-guided transurethral ultrasound ablation (TULSA) is a novel modality for minimally invasive ablation in patients with localised prostate cancer (PCa). A multi-national Phase 1 (30 patients) and subsequent Phase 2 (115 patients) study showed TULSA to be feasible, safe and well tolerated. However, technical viability and safety of salvage prostatectomy for those who failed TULSA is unclear. Herein, we report the feasibility and morbidity of salvage radical prostatectomy (sRP) post-TULSA.
Methods:
Four patients with biopsy-proven residual cancer following TULSA underwent open retropubic sRP within 39 months of TULSA. Peri-and post-operative morbidity were reported. Detailed histopathologic assessment is reported.
Results:
Median follow-up was 43 months after sRP. Mean operating times, blood loss, and length of stay were 210 min, 866 ml, and 3.5 days, respectively. Intraoperative finding of some fibrotic reaction of endopelvic and Denonvilliers fascia was characteristic. There were no perioperative complications. Whole-mount pathology sections showed one pT2b and three pT3a, suggesting under-staging pre-TULSA. Location of disease was compatible with persistent cancer mostly in the untreated peripheral safety region. One man received an artificial urinary sphincter. All men experienced erectile dysfunction responsive to treatment. Two patients with positive surgical margins had PSA progression requiring salvage radiation, with one requiring long-term androgen deprivation therapy.
Conclusions:
RP is a viable and safe salvage option if TULSA fails. Technical difficulty and perioperative morbidity were negligible and attributable to minimal peri-prostatic reaction from TULSA.
Hatiboglu et al, “Magnetic resonance imaging‑guided transurethral ultrasound ablation of prostate tissue in patients with localized prostate cancer: single‑center evaluation of 6‑month treatment safety and functional outcomes of intensified treatment parameters,” World Journal of Urology (2019)
Objectives
To evaluate the effect of intensified treatment parameters on safety, functional outcomes, and PSA after MR-Guided Transurethral Ultrasound Ablation (TULSA) of prostatic tissue.
Patients and methods
Baseline and 6-month follow-up data were collected for a single-center cohort of the multicenter Phase I (n = 14/30 at 3 sites) and Pivotal (n = 15/115 at 13 sites) trials of TULSA in men with localized prostate cancer. The Pivotal study used intensified treatment parameters (increased temperature and spatial extent of ablation coverage). The reporting site recruited the most patients to both trials, minimizing the influence of physician experience on this comparison of adverse events, urinary symptoms, continence, and erectile function between subgroups of both studies.
Results
For Phase I and TACT patients, median age was 71.0 and 67.0 years, prostate volume 41.0 and 44.5 ml, and PSA 6.7 and 6.7 ng/ml, respectively. All 14 Phase I patients had low-risk prostate cancer, whereas 7 of 15 TACT patients had intermediate-risk disease. Baseline IIEF, IPSS, quality of life, and pad use were similar between groups. Pad use at 1 month and quality of life at 3 months favored Phase I patients. At 6 months, there were no significant differences in functional outcomes or adverse events.
Conclusion
TULSA demonstrated acceptable clinical safety in Phase I trial. Intensified treatment parameters in the TACT Pivotal trial increased ablation coverage from 90 to 98% of the prostate without affecting 6-month adverse events or functional outcomes. Long-term follow-up and 12-month biopsies are needed to evaluate oncological safety.
Anttinen et al, “Feasibility of MRI-guided transurethral ultrasound for lesion-targeted ablation of prostate cancer,” Scandinavian Journal of Urology (2019)
Background:
MRI-guided transurethral ultrasound ablation (TULSA) has been evaluated for organ-confined prostate cancer (PCa). The purpose of this study was to assess the safety and toxicity, accuracy and short-term evolution of cell-death after lesion-targeted TULSA.
Methods:
This prospective, registered, Phase-I treat-and-3-week-resect-study enrolled six patients with MRI-visible-biopsy-concordant PCa. Lesions were targeted using TULSA with radical intent, except near neurovascular bundles (NVB). Robot-assisted-laparoscopic-prostatectomy (RALP) was performed at 3 weeks. Post-TULSA assessments included MRI (1 and 3 weeks), adverse events and quality-of-life (QoL) to 3 weeks, followed by RALP and whole-mount-histology. Treatment accuracy and demarcation of thermal injury were assessed using MRI and histology.
Results:
Six patients (median age¼ 70 years, prostate volume ¼ 60 ml, PSA¼ 8.9 ng/ml) with eight biopsy-confirmed MRI-lesions (PIRADS 3) were TULSA-treated without complications (median sonication and MRI-times of 17 and 117 min). Foley-catheter removal was uneventful at 2–3 days. Compared to baseline, no differences in QoL were noted at 3 weeks. During follow-up, MRI-derived non-perfused-volume covered ablated targets and increased 36% by 3 weeks, correlating with necrosis-area on histology. Mean histological demarcation between complete necrosis and outer-limit-ofthermal-injury was 1.7 ± 0.4 mm. Coagulation necrosis extended to capsule except near NVB, where 3 mm safety-margins were applied. RALPs were uncomplicated and histopathology showed no viable cancer within the ablated tumor-containing target.
Conclusions:
Lesion-targeted TULSA demonstrates accurate and safe ablation of PCa. A significant increase of post-TULSA non-perfused-volume was observed during 3 weeks follow-up concordant with necrosis on histology. TULSA achieved coagulation necrosis of all targeted tissues. A limitation of this treat-and-resect-study-design was conservative treatment near NVB in patients scheduled for RALP.
Anttinen et al, “Histopathological evaluation of prostate specimens after thermal ablation may be confounded by the presence of thermally-fixed cells,” International Journal of Hyperthermia (2019)
Purpose:
Prostate cancer can be eradicated with heat exposure. However, high and rapid temperature elevations may cause thermofixation giving the appearance of viable tissue. The purpose was to characterize the immunoprofile and evaluate the viability of prostate regions with suspected thermofixation.
Methods and materials:
A prospective, ethics-approved and registered study (NCT03350529) enrolled six patients with MRI-visible, biopsy-concordant prostate cancer to undergo lesion-targeted MRI-guided transurethral ultrasound ablation (TULSA) followed by radical prostatectomy at 3 weeks, to evaluate the accuracy and efficacy of TULSA with whole-mount histology as a reference standard. If ambiguity about complete necrosis within the ablated region remained after hematoxylin-eosin staining, viability was assessed by immunohistochemistry. Treatment day MRI-thermometry and 3-week contrastenhanced MRI post-TULSA were examined to assess ablation success and correlation with histopathology.
Results:
One patient presented with an apparently viable subregion inside the ablated area, surrounded by necrosis on H&E staining, located where temperature was highest on MRI-thermometry and tissues completely devascularized on MRI. Immunoprofile of the apparently viable tissue revealed changes in staining patterns suggesting thermofixation; the most significant evidence was the negative cytokeratin 8 staining detected with Cam5.2 antibody. A comprehensive literature review supports these observations of thermofixation with similar findings in prostate and other tissues.
Conclusion:
Thermally-fixed cells can sustain morphology on H&E staining. Misinterpretation of treatment failure may occur, if this phenomenon is not recognized and immunohistochemistry performed.
Based on the previous literature and the current study, Cam5.2 staining for cytokeratin 8 appears to
be a practical and reliable tool for distinguishing thermally-fixed from viable cells.
Bonekamp et al, “Twelve-month prostate volume reduction after MRI-guided transurethral ultrasound ablation of the prostate,” European Radiology (2018)
Purpose
To quantitatively assess 12-month prostate volume (PV) reduction based on T2-weighted MRI and immediate post-treatment contrast-enhanced MRI non-perfused volume (NPV), and to compare measurements with predictions of acute and delayed ablation volumes based on MR-thermometry (MR-t), in a central radiology review of the Phase I clinical trial of MRI-guided transurethral ultrasound ablation (TULSA) in patients with localized prostate cancer.
Materials and methods
Treatment day MRI and 12-month follow-up MRI and biopsy were available for central radiology review in 29 of 30 patients from the published institutional review board-approved, prospective, multi-centre, single-arm Phase I clinical trial of TULSA. Viable PV at 12 months was measured as the remaining PV on T2-weighted MRI, less 12-month NPV, scaled by the fraction of fibrosis in 12-month biopsy cores. Reduction of viable PV was compared to predictions based on the fraction of the prostate covered by the MR-t derived acute thermal ablation volume (ATAV, 55°C isotherm), delayed thermal ablation volume (DTAV, 240 cumulative equivalent minutes at 43°C thermal dose isocontour) and treatment-day NPV. We also report linear and volumetric comparisons between metrics.
Results
After TULSA, the median 12-month reduction in viable PV was 88%. DTAV predicted a reduction of 90%. Treatment day NPV predicted only 53% volume reduction, and underestimated ATAV and DTAV by 36% and 51%.
Conclusion
Quantitative volumetry of the TULSA phase I MR and biopsy data identifies DTAV (240 CEM43 thermal dose boundary) as a useful predictor of viable prostate tissue reduction at 12 months. Immediate post-treatment NPV underestimates tissue ablation.
Sundaram et al, “Therapeutic ultrasound and prostate cancer,” Semin Intervent Radiol (2017)
Abstract
Therapeutic ultrasound approaches including high-intensity focused ultrasound (HIFU) are emerging as popular minimally invasive alternative treatments for localized, low-to-intermediate risk prostate cancer. FDA approval was recently granted for two ultrasound-guided HIFU devices. Clinical trials for devices using MRI guidance are ongoing. The current level of evidence for whole-gland ultrasound ablation suggests that its clinical efficacy and adverse event rates including erectile dysfunction and urinary incontinence are similar to current definitive therapies such as radical prostatectomy and external-beam radiotherapy. Short-term data suggest that more focal therapy could reduce the rates of adverse events.
Ramsay et al, “Evaluation of focal ablation of MRI-defined prostate cancer using MRI-controlled transurethral ultrasound therapy with prostatectomy as the reference standard,” Journal of Urology 197: 255-261 (2017)
Purpose:
We evaluated magnetic resonance imaging controlled transurethral ultrasound therapy as a treatment for magnetic resonance imaging defined focal prostate cancer using subsequent prostatectomy and histology as the reference standard.
Materials and Methods:
Five men completed this pilot study, which was approved by the institutional review board. Prior to radical prostatectomy focal tumors identified by magnetic resonance imaging were treated by coagulating targeted subtotal 3-dimensional volumes of prostate tissue using magnetic resonance imaging controlled transurethral focused ultrasound. Treatment was performed with a 3 Tesla clinical magnetic resonance imaging unit combined with modified clinical planning software for high intensity focused ultrasound therapy. After prostatectomy whole mount histological sections parallel to the magnetic resonance imaging treatment planes were used to compare magnetic resonance imaging measurements with thermal damage at the cellular level and, thus, evaluate treatment and target accuracy.
Results:
Three-dimensional target volumes of 4 to 20 cc and with radii up to 35 mm from the urethra were treated successfully. Mean ± SD temperature control accuracy at the target boundary was −1.6 ± 4.8C and the mean spatial targeting accuracy achieved was −1.5 ± 2.8 mm. Mean treatment accuracy with respect to histology was −0.4 ± 1.7 mm with all index tumors falling inside the histological outer limit of thermal injury.
Conclusions:
Magnetic resonance imaging guided transurethral ultrasound therapy is capable of generating thermal coagulation and tumor destruction in targeted 3-dimensional angular sectors out to the prostate capsule for prostate glands up to 70 cc in volume. Ultrasound parameters needed to achieve ablation at the prostate capsule were determined, providing a foundation for future studies.
Chin et al, “Magnetic Resonance Imaging-Guided Transurethral Ultrasound Ablation of Prostate Tissue in Patients with Localized Prostate Cancer: A Prospective Phase 1 Clinical Trial,” European Urology (2016)
Background
Objective
Design, setting, and participants
Intervention
Outcome measurements and statistical analysis
Results and limitations
Conclusions
Patient summary
Trial registration NCT01686958, DRKS00005311.
Chopra et al, “MR Imaging-controlled transurethral ultrasound therapy for conformal treatment of prostate tissue: Initial feasibility in humans,” Radiology 265(1): 303-13 (2012)
Purpose:
To evaluate the feasibility and safety of magnetic resonance (MR) imaging–controlled transurethral ultrasound therapy for prostate cancer in humans.
Materials and Methods:
This pilot study was approved by the institutional review board and was performed in eight men (mean age, 60 years; range, 49–70 years) with localized prostate cancer (Gleason score 7, prostate-specific antigen level 15 mg/L) immediately before radical prostatectomy. All patients provided written informed consent. This phase 0 feasibility and safety study is the first evaluation in humans. Transurethral ultrasound therapy was performed with the patient under spinal anesthesia by using a clinical 1.5-T MR unit. Patients then underwent radical prostatectomy, and the resected gland was sliced in the plane of treatment to compare the MR imaging measurements with the pattern of thermal damage. The overall procedure time and coagulation rate were measured. In addition, the spatial targeting accuracy was evaluated, as was the thermal history along the thermal damage boundaries in the gland.
Results:
The average procedure time was 3 hours, with 2 or fewer hours spent in the MR unit. The treatment was well tolerated by all patients, and a temperature uncertainty of less than 2°C was observed in the treatments. The mean temperature and thermal dose measured along the boundary of thermal coagulation were 52.3°C 6 2.1 and 3457 (cumulative equivalent minutes at 43°C) 6 5580, respectively. The mean treatment rate was 0.5 mL/min, and a spatial targeting accuracy of 21.0 mm 6 2.6 was achieved.
Conclusion:
MR imaging–controlled transurethral ultrasound therapy is feasible, safe, and well tolerated. This technology could be an attractive approach for whole-gland or focal therapy. q RSNA, 2012
Chopra et al, “MRI-controlled transurethral therapy for localized prostate cancer”, International Journal of Hyperthermia 26(8): 804-21 (2010)
Abstract
Minimally invasive treatments for localised prostate cancer are being developed with the aim of achieving effective disease control with low morbidity. High-temperature thermal therapy aimed at producing irreversible thermal coagulation of the prostate gland is attractive because of the rapid onset of thermal injury, and the immediate visualisation of tissue response using medical imaging. High-intensity ultrasound therapy has been shown to be an effective means of achieving thermal coagulation of prostate tissue using minimally invasive devices inserted into the rectum, urethra, or directly into the gland itself. The focus of this review is to describe the work done in our group on the development of MRI-controlled transurethral ultrasound therapy. This technology utilises high intensity ultrasound energy delivered from a transurethral device to achieve thermal coagulation of prostate tissue. Control over the spatial pattern of thermal damage is achieved through closed-loop temperature feedback using quantitative MR thermometry during treatment. The technology, temperature feedback algorithms, and results from numerical modelling, along with experimental results obtained in animal and human studies are described. Our experience suggests that this form of treatment is technically feasible, and compatible with existing MR imaging systems. Temperature feedback control algorithms using MR thermometry can achieve spatial treatment accuracy of a few millimetres in vivo. Patient-specific simulations predict that surrounding tissues can be spared from thermal damage if appropriate measures are taken into account during treatment planning. Recent human experience has been encouraging and motivates further evaluation of this technology as a potential treatment for localised prostate cancer.
Chopra et al, “MRI-compatible transurethral ultrasound system for the treatment of localized prostate cancer using rotational control,” Medical Physics 35: 1346-57 (2008)